Research
In 2010, we began investing in studies into reducing and reversing the effects of Spinal Cord Injuries (SCI). Over a decade later, we have funded $1.9 million in SCI research. The discipline has made incredible progress, and leading scientists are hopeful about the prospect of finding a cure in the near future.
What is spinal cord injury?
The brain and spinal cord are your body’s central nervous system. The brain is the command centre for your body, and the spinal cord carries the messages back and forth from the brain. In a Spinal Cord Injury (SCI), the pathway between the brain and spinal cord is disrupted.
Why We Fund SCI Research
Most people understand a SCI to mean simply the loss of sensation or the ability to walk. But, for the majority of victims of Spinal Cord Injury, the implications extend much further. The spinal cord is indispensable to the regulation of the most important bodily functions including heart rate, sexual function, breathing, temperature, and bladder and bowel control – which means that some or all of these functions are often lost when it is damaged, depending on the injury.
SCI can happen to anyone at any time, and the dramatic consequences mean that it completely changes the lives of those affected, with outcomes for people in the developing world especially stark and often fatal. In spite of this, SCI research is staggeringly underfunded, with perceptions of the condition as ‘incurable’ and ‘not life-threatening’ leaving it side-lined in the medical research community.
That’s why, in 2010, Walkabout Foundation began investing in studies into reducing and reversing the effects of SCI. Almost a decade later, we have funded $1.9 million in SCI research. The discipline has made incredible progress, and leading scientists are hopeful about the prospect of finding a cure in the near future. Until recently, it was thought that regeneration of the spinal cord after injury was impossible. Now, thanks to this research, not only do we know this to be untrue, but we have also witnessed individuals regaining the ability to walk unaided. This opens the door to tremendous potential and hope for all those who have suffered a Spinal Cord Injury.
Shirley Ryan Ability Lab
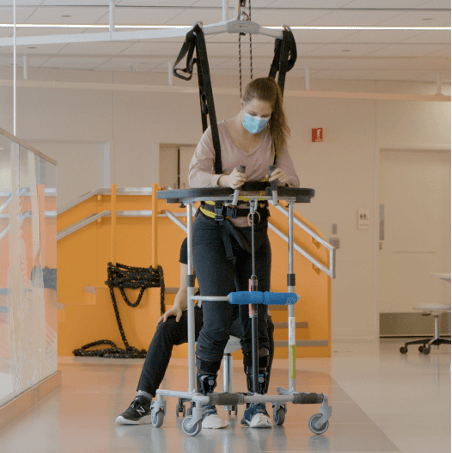
We are currently funding Northwestern University’s “Functional Restoration after Spinal Cord Injury by Hebbian and Transcutaneous Spinal Stimulation” study at the Shirley Ryan Ability Lab led by Dr. Monica A. Perez.
The study tests 15 patients with Spinal Cord Injuries, using Hebbian and transcutaneous electrical stimulations and exercise training in order to promote the recovery of function.
Dr. Monica Perez
Dr. Perez received a Ph.D. in physical therapy from the University of Miami School of Medicine. As a post-doctoral fellow, she attended the University of Copenhagen, where she studied transmission in spinal cord networks. She then completed a fellowship at the Human Motor Human Cortical Physiology and Stroke Neurorehabilitation Section at the National Institutes of Health, focusing on cortical physiology and plasticity.
Some of my best steps are my slowest steps. It is about slowing down and connecting with your body.
Amber Bruce
Participant in Shirley Ryan AbilityLab’s study
One morning, while getting ready for work, Amber experienced a C5-C6 incomplete SCI. She was taken to the hospital to undergo surgery and spent several months recovering in the hospital. During this time, she was determined to work hard on her recovery and researched medical trials that she could get involved with. With the help of her brother, they came across the Shirley Ryan Ability Lab and took off for Chicago. After 40 sessions of non-invasive neural stimulation, Amber finally took her first steps.
Previous Studies
The Big Idea – Christopher & Dana Reeve Foundation and University of Louisville
In 2017, in collaboration with the Christopher and Dana Reeve Foundation, UCLA and the University of Louisville, Walkabout committed $300,000 to a clinical trial studying the impact of epidural stimulation on 36 individuals with chronic Spinal Cord Injuries. The study evaluated the effectiveness of the treatment in improving cardiovascular function, standing and voluntary movement, as well as assessing improvement in sexual, respiratory and bladder function.The Big Idea also tracked the impact of this intervention in alleviating the financial burden of Spinal Cord Injury on individuals and the healthcare system.
To date, the 10 patients implanted with epidural stimulators experienced positive health outcomes. And in 2018, 3 out of the 10 patients regained the ability to walk.
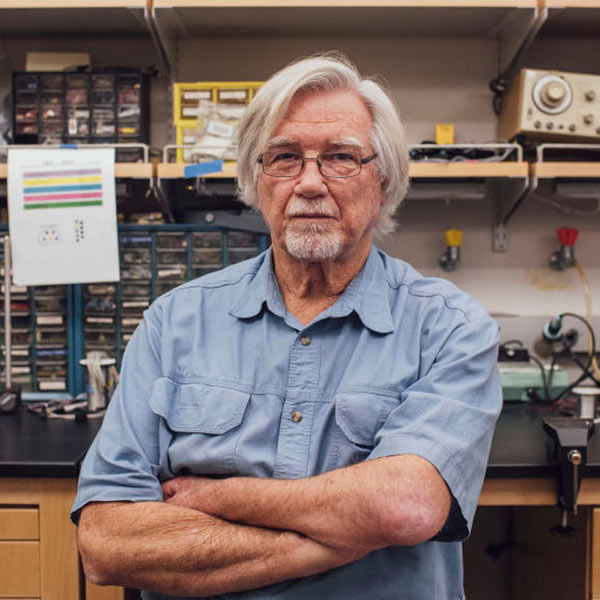
Transcutaneous Electrical Spinal Stimulation – Dr. Reggie Edgerton and UCLA
In 2016, we fulfilled our $1 million commitment to Dr. Reggie Edgerton’s lab at the University of California, Los Angeles. Thanks to our funding, in conjunction with the funding of only two other foundations, the lab was able to develop a groundbreaking treatment known as epidural stimulation, which completely redefined the future of the SCI research field.
Studies stemming directly from this incredible development enabled almost 20 participants to regain the ability to voluntarily move their own limbs, bladder and bowel control, sexual function, and the ability to sweat!
In September 2018, new research originating from Dr. Edgerton’s pioneering work saw three more individuals regaining the ability to walk, and a further two the ability to stand. These studies received widespread mainstream media coverage, and have underscored the promise of this technology as a viable treatment for Spinal Cord Injury.